Abstract
Introduction: Despite significant progress in the treatment of multiple myeloma (MM), the disease remains incurable and typically follows a pattern of multiple responses and relapses. In the relapsed/refractory MM setting (RRMM), outcomes for patients may be particularly discouraging. New treatments that are safe and effective are therefore of urgent need for this population. Since its FDA approval in 1998 for the treatment of rheumatoid arthritis, leflunomide has been used in over 300,000 patients worldwide. Leflunomide is hepatically cleared and has a favorable toxicity profile even when given over long periods. Its primary mechanism of action is inhibition of pyrimidine synthesis by targeting dihydroorotate dehydrogenase, thus achieving anti-proliferative effects on B and T lymphocytes. The anti-neoplastic potential of this agent has been studied in a number of pre-clinical tumor models.
Leflunomide's immunoregulatory action may be related to functional inhibition of CD4+ effector T cells, including Th17 cells as well as dysregulation of T regulatory cells (Tregs). We found that leflunomide-treated C57BL/KaLwRij mice engrafted with 5TGM1 cells had more robust expansion of CD8+ cytotoxic T cells and subsequent decrease of CD4+ Tregs compared to untreated mice. We have also noted that leflunomide impairs growth of MM cells at least partly through inhibition of PIM kinases and c-Myc signaling. We present here final results from a phase 1 study of leflunomide in patients with RRMM.
Methods: This single center, single agent, phase 1 dose-escalation trial was designed to determine the maximum tolerated dose of leflunomide in patients with RRMM. The trial implemented a modified rolling six phase 1 dose escalation design. The primary objectives were as follows: 1) to determine the maximum tolerated dose and recommended phase 2 dose of leflunomide; 2) to assess the safety and tolerably of leflunomide at each dose level by evaluation of toxicities. Leflunomide was administered at a loading dose of 100 mg daily for the first three days, then daily in 28-day cycles. The starting dose of daily leflunomide was 20 mg daily, with dose escalation in increments of 20 mg/day, up to 60 mg/day. Dose de-escalation in decrements of 10mg/day was planned.
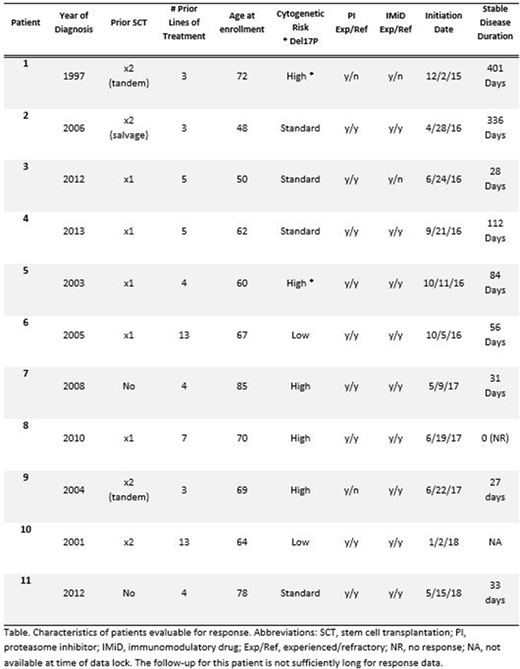
Results: A total of 12 patients have been enrolled starting in December 2015 and treated. The median age is 68 (range 48 - 85), and the median number of prior therapies is 5 (range: 3 - 14). Nine patients had prior autologous stem cell transplant. Double refractory (lenalidomide/bortezomib) disease was noted in 9 patients. High-risk cytogenetics were observed in 5 patients including 2 patients with del17p. All 12 subjects were evaluable for toxicity. One subject was not evaluable for response because of non-compliance. Of the eleven patients evaluable for response, the median number of cycles was 3 (range 1- 15). The median follow up was 177 days (range: 42 - 602). Three patients were treated on DL 1 (20 mg) and three on DL3 (40 mg) without incidence of DLT. At DL5 (60 mg), one patient had a DLT with grade III elevation of alanine aminotransferase; an additional three patients were enrolled at this dose level without further DLTs.
One out of 12 subjects remains on treatment, 8 patients were removed from study due to disease progression, two due to adverse events (bacteremia at 60 mg, possibly related to study drug and angioedema at 40 mg, not related to study drug) and one from noncompliance. The most common toxicities were hematologic. There were 4 patients with grade 1 or 2 neutropenia on the 20 and 40 mg dose levels and 1 patient with grade 4 lymphopenia on the 40 mg dose. Except for the DLT, all non-hematologic toxicities were ≤ grade 2.
Response: Although not all patients were treated at the 60 mg dose, a clinical benefit rate of 90% has been seen, with 9/10 achieving stable disease (SD). The median duration of SD among 9 patients thus far is 56 days (range: 27-401). In the five evaluable patients with high risk cytogenetics, four of them achieved a clinical benefit. Two subjects had SD lasting nearly one year or longer. In this small cohort, no association between dose and benefit was observed.
Conclusion: Leflunomide is a safe and well-tolerated oral option for patients with RRMM, with a clinical benefit from single agent dosing. On the basis of our preclinical work showing synergistic inhibition of MM using leflunomide, pomalidomide, and dexamethasone, we plan clinical testing of this drug combination.
Rosenzweig:Celgene: Speakers Bureau. Krishnan:Janssen: Consultancy, Speakers Bureau; Sutro: Speakers Bureau; Onyx: Speakers Bureau; Takeda: Speakers Bureau; Celgene: Consultancy, Equity Ownership, Speakers Bureau. Forman:Mustang Therapeutics: Other: Licensing Agreement, Patents & Royalties, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal